Postpartum + Chronic Illness Symptoms the Double Whammy
Roots and Truth
October 19, 2022

First of all I want to address those of you that clicked on this post in the midst of the struggle in the first few postpartum months. If this is you and you are desperately looking for help, click on this Symptom Directory where I curated a list of instagram pages and websites you can follow to find a larger community educating about postpartum feelings.
Second, I would encourage you to find a support group in your area. Google “therapist near me” OR call the front desk at your OBGYN or midwife group. Find one therapy office that you found on google (or that was referred to you) and ask if they know of a postpartum support group in the community. If you go—don’t take baby. (It is time to connect with adults who can speak!) Please find a trusted care taker to leave baby with during the hour and half meeting.
If you would like to start treating your whole body in its discovery and recovery, please connect with me by reading the following story. I have included a few personal care ideas at the bottom of this post. Thank you, for having a baby (if that’s your situation. I love you for what you are doing!
My Introduction:
If you haven’t read much about me, let me start off with a bang!
I’m Cami. I’ve been immersed in a near-death experience the past seven years. (Please…keep reading! I’ll explain!) It’s insanity to think about! I’ll try to explain more throughout this post, oh man, it is a lot to sort through and I’m trying to find my peace with missing so many good-young years of my life.
What does rummaging through past and backtracking do anyway? So I try not to retrace and regret the sad days. Even though this doesn’t seem possible, right now, to do.
Time has continued the last seven years. My husband and I have had to adjust in our marriage. I’ve been a parent to two boys, recently adding a baby girl! (Crazy! Right! Someone who feels like crumbling, can still create life!)
God, thank you for this body. It is a wonder, layered with issues. Filled with humanity and an everliving-soul! Disconnecting from many things in everyday-daily life has been good for me. The practice of resilience and reliance of God’s next offering is my new way of living.
My therapist said to me recently, “There are no atheists in a foxhole.” This parallels the Jungian perspective. When the back is truly against the wall. When the end seems inevitable, guiding fear leads to hope in a higher power.
Here is more of my story. If you want the beginning, and more background to my chronic health condition I suggest you read: The Beginning of My Health Journey
Intention and Conception
Have you ever read a book about someone who had a near-death experience? Or maybe watched a movie where the main character had a dream-like experience that may have changed the trajectory of their life?
What do you think when you hear their story? Did you (or do you) wish it was you living that experience?
Usually the main character in the narrative, recognizes the flip-side. The accident or life disconnect helps them question whether they really do want to live, and why. I recognize that many childbearing women have died during the process of giving birth. I do get out enough to see that every birthing mother has their own unique stories!! But I would like to share what has been unique in my story.
I watched my own mom’s postpartum experience after four babies. (She had six in total, I was her second.) With the exception of her second-to-last baby, I watched her bounce back. She acted like nothing big had happened. She breast fed with ease and continued her daily activities. She used the village as she raised six kids, but her energy continued through the years.
There is more of her story that I know she hasn’t told me. There were discouraging days as a young mother (but that’s not my story to share). I know that each delivery was not easy, but she clearly had full recoveries. Maybe there are more questions I need to ask her. Maybe I’m remembering things NOT as they are. (That is what I love about writing. It is allowing me time to question what I didn’t want to see clearly before.)
Something as routine as having a baby. Shouldn’t it be that…a routine? Not only routine, but a phenomenal occurrence that women have displayed since the beginning of Eve conceiving and birthing a child. But it is still routine. I wonder how many babies were born in the same hospital that day we received Weston, twenty, thirty, possibly?
Weston is my second child. My intention for conceiving him was to give my first son a sibling. Then maybe we would be done having children?!? Who knows—and so, NAIVELY, I conceived.
Conceiving wasn’t an issue for me with our first child4. It took me six months to conceive with our second baby. Risky, was the word that would best fit conception with Weston. I had chronic illness symptoms after giving birth to Scott. I agreed with labels and names like: fibromyalgia, “FibroFog” (fibromyalgia’s brain fog nickname) and chronic fatigue syndrome. All these symptoms were unexplained. I did see specialists that “ran tests”. I saw a rheumatoid arthritis specialist. Worked with a physical therapist, but natural muscle recovery didn’t seem to be occurring in my body. I played with diet to see if that could help with inflammation. I also saw a chiropractor regularly.
But I didn’t have a clue what pregnancy would do to my body the second time around. The days that remained, before Weston was born, I had a hard time walking. The tendons in my hips were ridged and tight. My aching legs inspired me to wear my hiking shoes into the delivery room. They were the most comfortable shoes that I had to walk in. And just in case you were wondering, delivering a child is NO walk in the park! I walked in totally prepared!

Weston’s birthday
Weston was born six hours after I entered the hospital. I delivered him with out pain medication. I did have an IV drip that had antibiotics and fluids to keep me hydrated. As my labor progressed I was disappointed that my ideal delivery wasn’t panning out. I started feeling ill right when I walked into the hospital in the middle of the afternoon. Then I felt the collapse. It happened in good timing because I was already checked in and sitting on my bed when I felt the wave of exhaustion and nausea. I had a vaginal infection. The medical team gave me a dose of Tylenol to relieve my fever and a drip IV with antibiotics.
We didn’t know the gender of the baby as we walked into our labor and delivery adventure. I gave birth to a healthy baby boy that day! I was strong. My body had enough energy to complete the task. I had the best team aiding me! And I loved how the day transformed into a magical completion of creation.
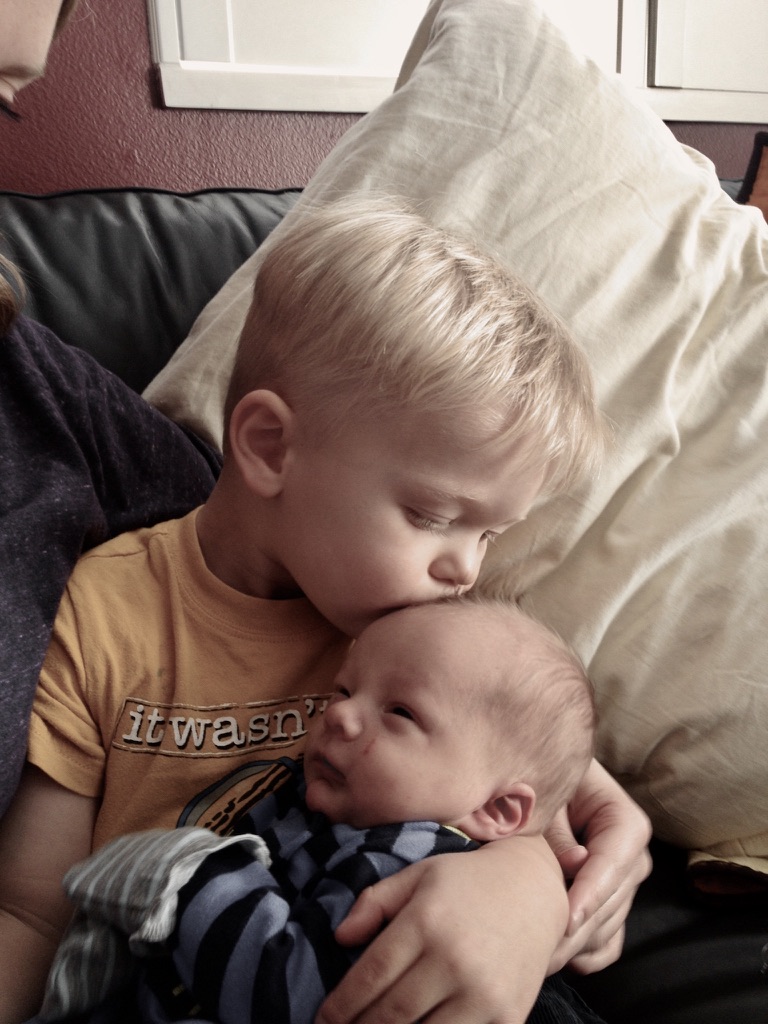
When I returned home around the first of March, Scott was able to meet his baby brother, Weston. He couldn’t remember his name for a few days. He called him “W” some of the time, and for some reason he call Wes, “Kiwi”. (I’m not sure why?) Scott was a month shy of turning three when Weston joined our family. He is a dynamic child, full of sass and energy. He was often by Weston’s side dressing him in random items that he had received or found in the house.
I continued caring for the new baby and my other busy buddy, but at six weeks the symptoms of fatigue and heaviness started setting in. I always had a headache and I could tell my pancreas wasn’t working well. I was already good at listening to my body. Mild blood sugar issues had always hindered me, but I had learned to care for it the best I could without heavily medicating. It was different this time. It was more extreme.


In my other post: The Begging of My Health Journey, I mention more symptoms that were happening at this same time. I also explained how I had to label what I was living for, because the daunting task of taking care of my body was HEAVY. I honestly didn’t know how I was going to return to health. The P.A. that I was seeing at the time told me that these were life-long issues. Although we were running blood work and trying to get to the root of the issue, there wasn’t much room in the space of HOPE.
The uniqueness of my story
One thing that was unique about my health challenges. I never got a diagnosis. There was never a treatable disease. I did treat an under-active thyroid with medication, but other then that, there wasn’t a medication I could take for my extreme blood sugar issues, or debilitating fatigue. It was labeled as “reactive hypoglycemia”. But why? What was happening?
At a low point in the first three months postpartum I started taking low dose birth control pills. I had tried taking birth control two times before, with the same symptom of feeling drained and depressed, accompanied by a lot of tears. After I cried for two days straight, I decided (for the third time) to quit the pills. It wasn’t worth feeling that way. My personal P.A. is a hormone specialist, and she gave me the best description of what was actually happening to my hormones as I took those pills, and why crying was a side effect. It was the first time from the medical community that I had received confirmation that I had made the right decision for my body. 1

This is important: Any time I had ever questioned the medical community before, or mentioned that the “pill” made me depressed, I was ignored or my feelings were denied. “Oh, no, taking the pill wouldn’t make you feel that way.” It was finally a relief to be validated and heard. I will continue to educate myself about this subject. It is a concern in the holistic health community.
My memory pockets in this whole postpartum period with Weston, are blurred. I know that we traveled some. I remember a family reunion we attended in the middle of the summer months. Weston’s skin was one big rash, so I remember seeing a doctor who is a pediatric allergist. I remember the shame that I felt when I went to Weston’s pediatrician, she saw my condition and strongly encouraged me to discontinue breast feeding. Oh yes, and the vacuum repair man. He called me and asked if we had a pet? He informed me that thin hair had ruined my vacuum. He had no idea that it was my hair because of the amount of thin hair he saw. I assured him that we didn’t have a dog.
I also remember questioning and reviewing everything I had ever known about my human body and general nutrition. My blood sugar was not regulating, my hair was thinning, my body was shrinking and my baby was begining to bleed on his scalp, because of his full-body rash.
Questions and dead ends
I started to wonder why my health challenges weren’t being explained. I had the best health care provider (I loved my P.A. and was being educated by her). She provided me with the most wonderful network, and even still “inflammation” was the answer that I continued to hear.
When Weston was eight months old I went to see an gastroenterologist. He looked at my blood work, then saw the crazy results. Liver and kidneys were being flagged. It alarmed him to see my face. He could visually tell that my muscles were shrinking. He ordered a liver biopsy, that I scheduled and followed through with.
When the results were returned we scheduled a special meeting because something had been discovered from the biopsy. The nurse didn’t tell me over the phone, but she called and asked me to come into the office. After a forty minute drive, my husband taking the afternoon off from work, and leaving our boys at neighbors for the afternoon, I sat in the G.I.’s office again. We heard from a Nurse Practitioner (who assisted the doctor) that they had found, “A little inflammation in the liver.”
My husband was SO bugged! “Really, you couldn’t have told us that over the phone?” He said as we drove home. I think it is important to add, I really did like the doctor. He was totally overworked and overbooked. I was fine seeing the assistant to receive that information. But it was creating an enormous amount of stress in my life to keep up the schedule into my personal investigation. so…
Reaching out into a larger community
As I sat waiting to see the gastroenterologist in September, I had plenty of time to look around the waiting room. There were sick people surrounding me. I was on time, but waited an hour that day for the doctor to see my depleted face. I wasn’t alone in waiting. Everyone else wanted see the doctor to have their symptoms explained, or their medication refilled.
At my follow up in November, after my liver biopsy, I finally saw the doctor again. He actually had time to talk that day. The last four months I had spent researching. When he entered the room I showed him one of the “text book” style books I had been reading that explained how to heal from the inflammation. I asked he if he had heard of it. Then I explained what I was doing with diet change.
Of course he hadn’t read it, he is a super busy man, but this specialist gave me a gift that day. The answer he had was, “I don’t know what is wrong with you. But I do know that you’re a smart girl. You’re going to figure it out.”
His humility was received. I walked out of the office with a key of empowerment. A dead end in a way that led me to believe that there was an answer for me, but I didn’t need to keep spending my time and money in this specific place.
So I kept reading and receiving more keys, to different avenues.

Where did I get the healing book “text book” in the first place?
Here is one massive clue to parenting, healing, researching, education, or really anything. Learning how to reach out and ask for help has been an invaluable skill!
On a Sunday when I was out of town, a women in my neighborhood shared a story at church. I heard second hand of her testifying that God was helping her heal from a horrific pregnancy and chronic illness condition mash up (kind of like mine). Someone in my neighborhood mentioned her story to me, so I called her. The conversation went like this. “Hi, this is Cami, I don’t really know you yet, but someone told me that you were on a special diet to help heal your body. Would you mind telling me what you are doing?”
We set a up time that I could meet with her at her house when her kids were at school. She shared with me her knowledge and I bought the huge similar to a “text book”, book. I read the book all the way through two times. The section about blood sugar issues I read over and over again. I followed the book’s suggested protocols. The recipes linked to the book’s protocols, were not easy to make, but I made them anyways. This book was not the information that could help me long term, but it was a stop on my way to the next avenue.
This women and I continued to connect through recipes and healing strategies. She has been a gift to me, and I hope I to her. But the book she gave me kept me questioning. My extreme blood sugar swings weren’t going away.
Adapting
The postpartum period adjusting to a new baby was easy with my second. I had given part of my life for this baby, so I valued him as a high-priced gem. He was happy and scabby, but at least he was happy! And he was easy to care for.
As I have observed my babies’ growth and studied human behavior, I think it is kind to say that most adults are set in their ways when they bring on a child. Good thing most of us have months to prepare bedrooms, minds and hearts for this change, but still the majority of adults can’t progress and adapt at the rate babies are adapting. In the first year the feeding schedule changes at least six time. Generally at the six month mark solids are introduced, but a variety of foods should be given. In the first year a child is completely dependent at the beginning and then is crawling or walking away by the end of the it. Sleeping schedules change at least four times.
And what does a parent have to do? —Adapt!
This is not easy, especially if you’re doing it for the first time! Why, because it takes behavioral change.
Through the months after having Baby Weston, I had to study and change for myself. I stayed inside most of the time because I was weak. I was also breastfeeding and deep diving into research (at the same time). I had a full time job caring for his skin, cooking whole-food meals and attending the doctors appointments that I was scheduling.
I gave my life away to physical and mental care that first year. I made it a priority to find a therapist that would listen to me. Becky specialized in grief, loss and the pain of suffering that accompanied it. She was a good match for me on this stop of my personal discovery path.
I was adapting constantly. I personally changed my diet 3 times that first year. The baby kept eating what I ate. I didn’t make special food for him.2 I could usually mash up what I was eating (when he was old enough to eat solid foods).
The following chart illustrates how I moved forward through my change. I couldn’t control the circumstance, but with intention I was able to change.
I developed this chart to illustrate the structure that I have followed through my investigative journey. This was written and intended to be used by the larger community trying to heal from a chronic illness or condition. For this post I am illustrating what I did postpartum to help me through the first year after giving birth to Weston. A more complete chart can be found in this blog post.
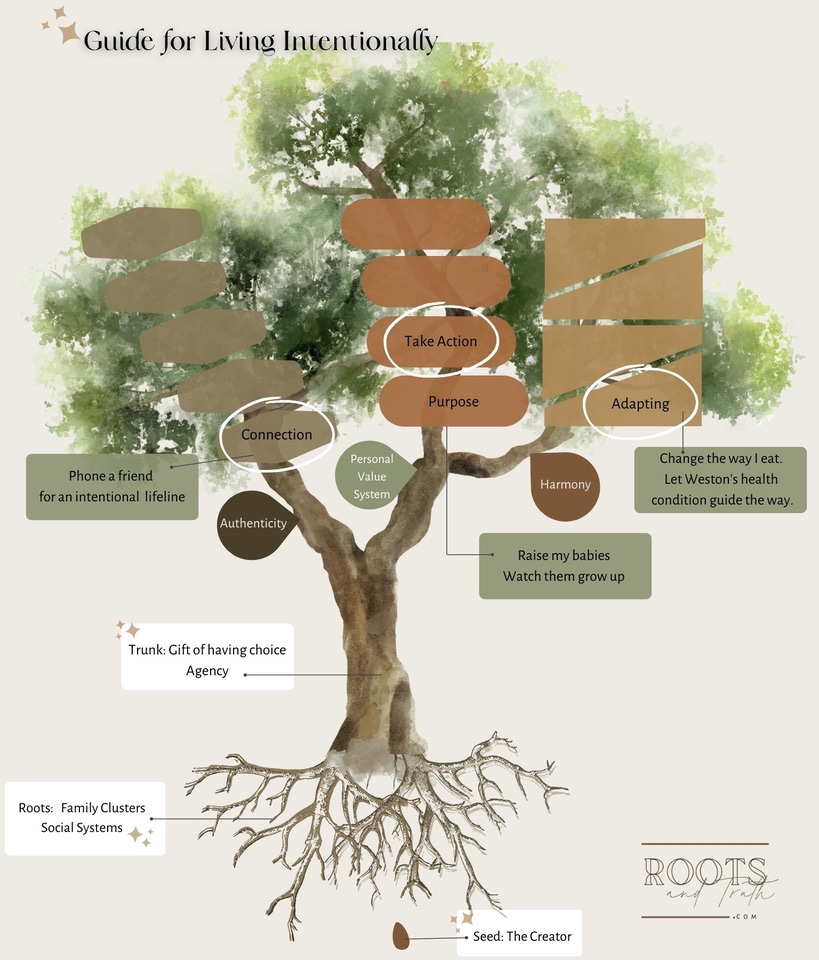
Actionable steps that I decided to take the first year:
- I continued to breast feed my baby to connect on a non-verbal level. (Read at the end of this post. I wrote about it in more detail.)
- I continued seeing the Physician Assistant that I had previously establish care with. We continued our investigative work. I had new labs done every six weeks.
- I called a neighbor and asked her about the healing diet she was on. I bought the book that she was reading and studied it and applied what it taught.
- I saw multiple specialists.
- I continued to bathe Weston and use a steroid cream, that I had received from the Allergist M.D., to help with his physical inflammation.
- I started therapy to have a sounding board in the midst of all the change.
I was determined to watch Weston grow up. For this period of time, he was my reason for behavioral change. He kept me going. With all the complexities of living intentionally; all the agenda’s that I can’t control; all the circumstances that I don’t have answers for, I did not live this way consistently.
Actually, I was stuck in the house most of the time as a result of low energy, and loss of muscle mass to carry me around. By the end of the year, I felt like a hollow frame. If I knew how to explain my inner feelings, and if knew the resource of Polyvagal Theory in this time frame, it would have been wonderful!
There was more information available that is filled with a mammalian view, and a whole lot of love! Let me explain!
Anxiety that accompanies instability
When my personal physician was looking at my blood work we could see that there was issues happening in the endocrine system. This system includes the thyroid, adrenals and pancreas. The root cause of why the blood work was flagged was unknown. But with so much inflammation the adrenal glands were pumping adrenaline excessively.
Along with cortisol adrenaline is a gift, it gets us out of bed in the morning. It creates thrill when we get to sing or perform in front of a crowd. It is a chemical messenger for the body. It communicates to the body to keep going. This chemical reaction helps us get out the way of danger. It keeps us safe!
Many mothers suffer with adrenal fatigue, and they need large periods of rest to tell the body to stop pumping out these chemicals continuously.
REST—Not always consistent with a new baby. Or with multiple kids around.
Although my adrenals were taxed postpartum, this in not the case for everyone who just had a baby. It is case by case. (I had underlying issues as well.)
In my specific case ANXIETY was not ruling my life. My body was in self protective mode, or shut down most of the time for the first year.
I can explain it better now using the information that I have gain after studying Polyvagal Theory4
More about the natural cycle of moving through stressful experiences
Remember how I began the article. I’ve been stuck in a cycle of not feeling physically capable of living. Every time I have tried to link the clues to escape this cycle, floods of anxiety come next and then I return to a frozen state of constriction. This tightening and locking up is showing up in my body as a physical symptom. My nervous system has been stuck in a “Sympathetic” pattern for far too long. “Sympathetic” is more easily explained as the “Fight or Flight” response.
During the postpartum period, if there was any events that would be described as “violating” during the birth, during conception or previous events, that sympathetic reaction of fight or flight may arise. Why?
To get your body, or your baby to a safer place. It is energy that needs to be explained (by you). So please find a safe place to voice any concern that you have about your body, or your growing baby.
Here is the beautiful cycle that Polyvagal Theory teaches that I found true through the moments of my birthing processes.
>>>If this list triggers you in anyway (in other words makes you blame or shame your experience) then stop reading and scroll to the bottom of the post to the heading titled: “What steps can I take?”
The natural cycle specifically during the birthing process should include:
- The body’s complex and unique system utilizes hormones and adrenaline to begin the contract and releasing mechanisms in the body as the baby descends into the birth canal
- A near-death experience during the “transition period” where the brain can’t discern if the body will live through the experience, or die during the process.
- The actual birth and delivery of the placenta. It defines the event as resolved—the crowing moment! The body naturally feels excitement, joy an increase of attachment.
- A period of shaking5, possibly throwing up. This is actually a part of the process. It is the body’s way of getting rid of excessive adrenaline. It also sends a message to the brain via the vagus nerve that all is well. The movement is mobility that signals a to the brain to anticipate a period of safety.
- Calming down, resting, warming and returning the nervous system to regulation. This feeling is accompanied by feelings of contentment, peace and calm. Tools can be used to reach that state of regulation. A list of tools may include (but is not limited to): A warm blanket, the new baby on the chest, a snuggle from your companion or birthing partner.6
If the steps in this cycle were missed or left incomplete, feelings of panic, anxiety, or in my case shut down and tightening may persist. Some may label this as birth trauma. Healing from birth trauma is possible, it is important to know that you are not alone if the sequence in this cycle was not reached in anyway.
Keep letting the excessive energy escape through words and tears, instead of hiding the feelings of disappointment or shame. (A trained-licensed therapist may assist you during this season of life.)
If this was not the case for you, keep reading…I have one more point to make.
The positive side of anxiety
The reason that I include Stephen Porges research on the vagus nerve is to teach that anxiety (or feeling into your sympathetic nervous system) is actually a better place to feel then the feelings of disconnect or shut down that I previously explained. If you want to read more on dysregulation and shutdown, I sourced more in this post: Digging Into Depression Productively.
The vagus nerve runs from the base of the brain through the body and connects near the end of the spine. It receives messages from the body and sends those messages to the brain. If there are past experiences that have not been released through this simplistic action of movement as a form of energy, then trauma typically stays stuck, as well as unresolved. When I use the word energy, I actually mean that the body physically needs movement to resolve. In the case of childbirth that shaking feeling, the stimulant of shock, resolves of the intense emotions that the body has been experienced.
This is not a shameful subject for me. I would rather people be educated on the proper steps to work through birth trauma, then to stew in them for decades. With Weston’s birth I completed the intense cycle of events. The result was feeling fulfilled and empowered after giving birth! But this was not the case with my first son. I had not completed the trauma cycle and was extremely angry with the unsupported team that accompanied me. I wrote about his birth in this post.
I was still suffering from the effects of that birth while I was pregnant with Weston. It actually took me eight years to feel that it had healed and resolved. I think this unease has contributed to my chronic pain, as well as other factors.
With Weston I didn’t have underlying shame about his birth, but I was overwhelmed with the symptoms I was facing after his birth. My body was so low, it was in an autonomic nervous system state to conserve energy.
My thoughts about my health were obsessive. It was my reality that was fogging my head space. Ruminating in fearful thoughts can also be a hard to communicate with those close to you. It may cause you to close off relationships if the pattern isn’t recognized. With this visual, do you see how an obsessive cloud can hinder my ability to be intentional?
I would attribute my obsessive behavior that I was displaying trying to figure out my health condition as a polarization issue, more than an anxiety issue. You can read more about polarization in this post.

It is healthy to have a phase of time to stay in, and stay away from family and friends after giving life to another living soul. There needs to be uninterrupted resting time. There is a period of time it takes to figure a new schedule out. It is safe to keep a vulnerable little body free from viruses that may creep in. Setting boundaries and allowing time to acclimate is beneficial!
So when is the balance unhealthy? Here are some questions that you can ask yourself.
- What advice would you give someone, about your situation, if you were the one on the outside looking in?
- What is your current intention? (Remembering you can not return to your past experience to fix it.)
- Refer to the tree visual above. Remember where you came from. That seed that was designed perfectly. You are valued and worthy!
- When you look at a child, does he or she reflect anything back to you? What do you see? Possibly the tension you are feeling through this phase reflects something that is surfacing that you need to see.
The miracle
My obsession on saving my body was obviously forefront. Is that the wrong thing to be obsessed about?!? I don’t think so! But let me say it boldly, my ways were of eating were extreme!
Even though I was displaying polarity (and extreme behavior), I was low and conserving energy anywhere I could—always weighing mentally with a cost to benefit analysis. I was in the “foxhole” so to speak. I was going through a process that required reaching for something higher and holier. It was a blessing, but in foresight and hindsight it was more extreme. You can read about my second year postpartum in this post: More About Me and the Process of Cleaving
The aforementioned post dives more into the spiritual nature of my suffering.
As I began the post you are now reading, I mentioned my current suffering. I now have a name for it. It is called “constriction” or as I can describe it in layman’s terms, instability and a seemingly inability to release what is inside of me. It is a side-effect of what has been patterned in my autonomic nervous system.
In this space, where does God come in? Or the Creator? As I named it in the Guide for Intentional Living.
For me, I seek oxygen and light. Whole foods that add water and minerals to my body and mind. When these things are consistent I have enough to continue. I am still in physical pain. But, I acknowledge my pain as a guiding light.
What if ignored the problem and kept dousing my pain with shame or continuously hiding? (These are patterns that I have displayed previously. Remember my confession in the beginning of this post?)
For me, it is worth receiving incremental light. So what is in it for me?
I am learning as I’m writing. It is an empowerment practice for me. And hopefully some of these resources can help you.
Reviewing this article: What steps can I take?
- Confide in someone who will acknowledge what you are going through. OR ask a friend in this way, “I’m feeling like ___________ was robbed from my body. Have you ever felt that way?”
- Talking to a partner about a specific fear can not only create relief, but help develop deeper connection. A conversation may look something like this: “I keep thinking that this is totally an irrational fear, but what if our baby got this _________________(insert disease) and he/she…” (If you need a specific example about speaking truth, please read: More About Me and the Process of Cleaving)
I’m not going to put fears or words into your mouth, but hopefully you get the point.
- Please review if this child was planned. If the pregnancy was planned, what expectations did you have through conceiving?
- Please review with a trained therapist or somatic practitioner if there is a feeling of an incomplete pregnancy, including a miscarriage, an ectopic pregnancy, an abortion, a stillborn birth, a birth defect effecting your child, even a child that was sent to the NICU immediately after birth. If you still feel a void or something that still feels incomplete please receive help. (My promise to you is, there is healing through connection and self compassion.)
- If you feel like you are disconnecting from those around you, it may be likely that Somatic Therapy may be a right fit for you. This is a course online that is under $100 but has helped me immensely.
- If none of these ideas or resonating, set an intention for your self care. A cared for mama is an all around better mother!
Resources and links
An introduction about the vagus nerve. And simple movements you can do at home.
More about being informed and naturally taking care of your reproductive health (specifics on birth control)
- Body Literacy Library: A women’s body awareness and larger options resource page
During the process of growing the child and accounting for the amount of resource it takes to deliver, most likely magnesium stores are depleted. This website is an educational resource and a source to buy a quality soaking magnesium. Soak your feet regularly to restore this most vital mineral, or pour some in the tub and soak.
The following is a comforting recipe I made over and over again during the first two years postpartum Weston. It is a warm weekend porridge. It reminded me of creamy wheat. But without the wheat. I wasn’t metabolizing grains well because of my pancreatic health. This porridge is made with coconut milk, spaghetti squash and tapioca pearls. When I make it I love to serve it with fruit and honey and almond milk.
Weekend Spaghetti Squash Porridge
This is a “No Grainer” recipe that I have used every fall and winter as a breakfast and as a comfort food. I would compare it to a creamy wheat breakfast porridge.
Potassium is a mineral that is crucial to add more of when dealing with chronic illness. To increase the amount of potassium I always top my bowl with potassium rich fruits. Some suggestions include, but are not limited to: wild blueberries, bananas, dates, peaches, pears, or mixed berries.

Ingredients
- 6 cups water (divided)
- 1 cup tapioca pearls
- 4-5 cups cooked spaghetti squash (one small squash)
- 1 14 oz. can coconut milk
- 1 teaspoon salt (optional)
- 1 tablespoon cinnamon
- 2 tsp. vanilla (or 1 inch of vanilla bean, sliced open lengthwise)
Instructions
- In a small bowl combine the tapioca pearls and 1 cup of water. Let soak for 10 min.
- With a spoon, scoop the cooled squash out of its skin. Combine the squash and five cups of water in the pot on medium heat. Break up the strands with an emulsion blender.
- Add the soaked tapioca pearls, coconut milk, salt and cinnamon. Bring it the mixture to a simmer.
- Turn the stove to low heat until the pearls look clear. This takes about 20 minutes.
- Add the vanilla, stir until combined.
- Serve with seasonal fruit and top with honey if desired.
Notes
This is nice to make on the weekend because the squash can be baked on Saturday, make the porridge on Sunday, then eat on the batch all week by quickly heating in the morning.
If an emulsion blender is not available, put the cooled spaghetti squash on a cutting board and chop with a chef knife until you have the strands chopped into 1/4 inch sections. Add the chopped squash into the pot of with water and continue with the list of instructions listed in the recipe.
Tags
- I felt like every time I had a baby, instead of receiving love at the hospital from the midwife or doctor, I was peppered to think about my next decision for contraceptive. Both times, I caved in, tried the “low low” dose and both times felt so discouraged on the drug. I received validation the night, recently, that I watched “The Business of Birth Control” by BOBB studio. I felt part of a grander society of womanhood that had listened to the creation of their body, and didn’t feel well on the pill. As a result they started questioning. But I could also tell that society at large weren’t/aren’t questioning the doctor or general practitioner and are on the medication for reasons like PCOS (Polycystic Ovarian Syndrome), acne, and irregular periods, as well as pregnancy prevention. What seemed to be “hormone” related issues were being blanketed by these pill. Often prescribed by a physician that hadn’t even ran blood work, reviewed scans or looked else where for an underlying issue. So what’s the truth? In my opinion the truth of these before mentioned issues are linked to viruses, overgrowth of negative bacteria, environmental toxicity and stress. Things we don’t take into account, but our bodies don’t react well with because they aren’t natural. Environmental toxins may include (but are not limited to fragrances (perfumes, lotion, wall plugins, laundry detergent ect…), the overuse of glyphosate on our commercially grown food (even the weed killer that is often used in our own yards, water that has been contaminated, breathing dirty air. So what can we do? Remove some of the things, that we can control, away from our bodies. Consider following someone who is researching and teaching about environmental toxins. Justingredients.us is my favorite educator. Remove some of the invaders or pollutants that are already in the body with magnesium soaks. (There is a resource listed above.) Start the morning with a glass of lemon water, or water and magnesium glycinate. This could be such a blessing for an overtaxed body. If this is too much for you, start reading, slowly about this subject. Anthony Williams books resonated with me when I was going through my learning curve.[↩]
- If you are interested in this topic at all, here’s a title to a book that may be helpful: Infant Led Weaning by Gill Rapley PhD https://www.amazon.com/Baby-Led-Weaning-Completely-Expanded-Anniversary-ebook/dp/B07H3GS91K/ref=sr_1_7?crid=PKVGM4B6XR9Y&keywords=infant+led+weaning&qid=1665802037&qu=eyJxc2MiOiIyLjQ2IiwicXNhIjoiMS42OSIsInFzcCI6IjEuMjIifQ%3D%3D&sprefix=infant+led+weaning%2Caps%2C158&sr=8-7[↩]
- Petersen, Cami, Guide For Intentional Living: Taking Action Image, 2022, https://rootsandtruth.com/postpartum–chronic-illness-symptoms-the-double-whammy/(opens in a new tab)[↩]
- In 1994 [Stephen Porges] proposed the Polyvagal Theory, a theory that links the evolution of the mammalian autonomic nervous system to social behavior and emphasizes the importance of physiological state in the expression of behavioral problems and psychiatric disorders. The theory is leading to innovative treatments based on insights into the mechanisms mediating symptoms observed in several behavioral, psychiatric, and physical disorders. Source:https://www.stephenporges.com/about[↩]
- You might experience some severe shaking and shivering after your placenta is delivered. This is a common symptom and not a cause for concern. Source: https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/third-stage-of-labor/[↩]
- If you tore or had an episiotomy, you’ll get an injection of a local anesthetic before being sutured. You may want to hold your newborn while you’re getting stitches – it can be a great distraction. If you’re feeling too shaky, ask your partner to sit by your side and hold your new arrival while you look at him. [this assists with co-regulation] source: https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/third-stage-of-labor/ [↩]

Leave a Reply Cancel reply
© roots and truth | All rights reserved | Site design by linsey rhyne co.

Great post.
Thank you for reading!
I like the efforts you have put in this, regards for all the great content.
Thank you for reading!
Wow, this blogger is seriously impressive!
I appreciate your creativity and the effort you put into every post. Keep up the great work!
Thank you for being here!